If you know a veteran struggling with post-traumatic stress disorder (PTSD), you might feel unsure of how to help. Maybe they seem distant, on edge, or carrying an invisible weight. PTSD isn’t just about bad memories—it’s a condition that can impact every part of a person’s life, making it difficult to connect with others, hold a steady job, or even feel safe in their mind.
At The Last Resort Recovery Center in Austin, Texas, we’ve worked with countless veterans who feel trapped by their trauma. Our men-only treatment programs create a space where they can begin to heal alongside others who genuinely understand. Through evidence-based therapy, equine-assisted treatment, and experiential healing, we help veterans regain control of their lives.
If you’re looking for ways to support a veteran with PTSD, here’s what you need to know.
Understanding PTSD in Veterans
Post-traumatic stress disorder (PTSD) is a mental health condition that can develop after experiencing or witnessing a traumatic event.[1] It’s particularly common among veterans, whose service may expose them to intense and life-threatening situations. PTSD goes beyond temporary stress or anxiety—it’s a persistent condition that can disrupt daily life, making it difficult to regulate emotions, maintain relationships, or feel safe in familiar environments. While the effects of PTSD vary from person to person, specific patterns of symptoms often emerge.
PTSD doesn’t follow a set timeline. Some veterans begin experiencing symptoms immediately after service, while others go years before realizing the extent of their struggles. The causes of PTSD vary widely—combat exposure, military sexual trauma, life-threatening experiences, or even the cumulative stress of service can all play a role. Regardless of the cause, PTSD can disrupt every aspect of a veteran’s life, from their relationships to their sense of security in the world.[2]
1. Reliving the Trauma
One of the most distressing aspects of PTSD is the way traumatic memories resurface. Flashbacks, nightmares, and intrusive thoughts can make it feel like the past is happening all over again. These episodes may be triggered by sights, sounds, or even emotions that remind the veteran of their trauma. In some cases, the body reacts as if it is back in danger, leading to physical responses such as sweating, a racing heart, or panic attacks.
2. Avoidance
To cope with painful memories, many veterans develop avoidance behaviors. This can mean steering clear of places, conversations, or even people that remind them of their trauma. In some cases, avoidance extends beyond specific triggers and leads to emotional withdrawal from loved ones. A veteran struggling with PTSD may seem distant or uninterested in activities they once enjoyed, making it difficult for friends and family to maintain close relationships with them.
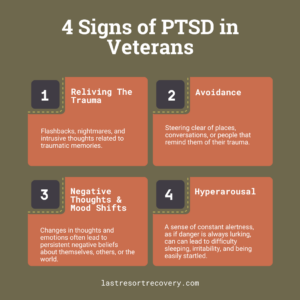
3. Negative Thoughts and Mood Shifts
PTSD can alter a veteran’s thoughts and emotions, often leading to persistent negative beliefs about themselves, others, or the world. Feelings of guilt, shame, or unworthiness are common, even when the veteran is not at fault for what happened. Many experience emotional numbness, making it difficult to connect with others or feel joy in situations that once brought happiness. Over time, this shift in thinking can contribute to depression, self-isolation, and difficulty trusting others.
4. Hyperarousal
For many veterans, PTSD creates a sense of constant alertness, as if danger is always lurking. This heightened awareness can lead to difficulty sleeping, irritability, and being easily startled. Minor, everyday occurrences—such as sudden noises or crowded spaces—can trigger an intense fight-or-flight response. At The Last Resort, we’ve seen firsthand how veterans struggling with hyperarousal often feel like they can never fully relax, even in safe environments. Through evidence-based therapies and a structured approach to recovery, we help them reprocess their trauma and develop strategies that reduce this constant state of high alert.
Related: Veterans Drug Rehab in Austin, TX
How to Support a Veteran with PTSD
Supporting a veteran with PTSD isn’t about having all the correct answers—it’s about showing up and creating a safe space where they feel understood. While you can’t erase their trauma, your support can make a meaningful difference in their healing process. The key is to approach every interaction with patience, respect, and a willingness to listen. Even small gestures, like being present without pressuring them to talk or learning more about PTSD on your own, can help them feel less alone. Here are some ways you can offer support that truly resonates.

1. Let Them Lead the Conversation
You don’t have to know the perfect thing to say. Trying to dig too deep too soon can push them away. Instead of asking, “What happened?” or “Are you seeing a therapist?” let them know you’re there without pressure.
Try saying:
- “I know things have been tough. Whenever you want to talk, I’m here.”
- “You don’t have to go through this alone. If there’s anything I can do, just let me know.”
At The Last Resort Recovery, we see the power of peer support every day. Veterans often feel most comfortable opening up to others who’ve been through similar struggles.
2. Educate Yourself About PTSD
Imagine helping someone afraid of swimming. You wouldn’t just tell them to “get over it” or throw them into deep water. Instead, you’d learn about their fear, offer them a life jacket, and maybe even take a swimming lesson yourself. PTSD is similar—the more you understand it, the more helpful you can be.
- Read up on PTSD through reputable sources like the VA or the National Center for PTSD.
- Attend family support groups or workshops designed for the loved ones of veterans.
- Learn about triggers—things like loud noises, crowds, or even anniversaries of traumatic events that can cause distress.
3. Encourage Treatment Without Pushing It
Many veterans hesitate to seek help because they don’t want to be seen as weak. They might also feel like therapy won’t work for them or that no one will truly understand what they’ve been through.
Instead of saying, “You need to see someone,” try:
- “I’ve heard about programs that actually help veterans work through PTSD in a way that makes sense for them. If you ever want to check it out together, I’d love to help.”
- “You deserve to feel better. I know it can be hard to reach out, but I’ve seen others find real support, and I want that for you too.”
At The Last Resort Recovery, we offer more than just traditional therapy. Our programs blend trauma-focused treatments, equine-assisted therapy, and experiential healing in a way that resonates with veterans.
4. Help Them Find Healthy Coping Strategies
Veterans with PTSD often turn to alcohol, isolation, or risky behaviors as a way to cope. If your loved one is struggling, help them find better alternatives.
- Encourage physical activity – Exercise can be a powerful tool for managing PTSD symptoms. A simple hike, weightlifting session, or even stretching can help release tension.
- Introduce mindfulness techniques – Deep breathing, meditation, or even listening to calming music can help regulate emotions.
- Suggest outdoor experiences – Nature has a grounding effect. A camping trip, fishing, or even a walk in a quiet park can help clear the mind.
At The Last Resort Recovery, we integrate fitness therapy, equine therapy, and outdoor activities into our treatment programs because we’ve seen firsthand how incorporating physical activity—whether it’s hiking, weightlifting, or working with horses—helps veterans reconnect with their bodies and manage PTSD symptoms in a healthier way.
5. Know When It’s Time to Seek Immediate Help
PTSD can increase the risk of depression, self-harm, and suicidal thoughts.[3] If a veteran you care about starts talking about feeling hopeless, withdrawing completely, or engaging in reckless behavior, take it seriously.
Signs of a crisis include:
- Expressing feelings of hopelessness or being a burden.
- Increased substance use or risky behavior.
- Completely shutting down or isolating themselves.
Resources for Immediate Help:
- Veterans Crisis Line: Dial 988, then Press 1
- National Suicide Prevention Lifeline: 1-800-273-8255
- VA Mental Health Services: www.va.gov
If you’re unsure how to handle the situation, contact a mental health professional or seek guidance from The Last Resort Recovery Center. We specialize in helping veterans recover from addiction, PTSD, and other co-occurring conditions.
Related: Substance Use Disorder Treatment in Austin
What Are Positive Coping Strategies for PTSD?
The best way to manage PTSD effectively is by using practical, evidence-based coping techniques that help veterans regulate emotions, process trauma, and regain control.[4] The most effective strategies come from cognitive behavioral therapy (CBT), dialectical behavior therapy (DBT), somatic experiencing, and acceptance and commitment therapy (ACT).

- Cognitive reframing (CBT) – PTSD often distorts thoughts, making veterans feel hopeless or stuck. Challenging negative beliefs and replacing them with balanced perspectives can shift how they process trauma. For example, instead of thinking “I’ll never be normal again,” reframing turns it into “Healing takes time, but I am making progress.”
- TIPP method (DBT) – This fast-acting distress tolerance skill calms intense emotions through Temperature change (cold water or ice packs), Intense exercise, Paced breathing, and Progressive muscle relaxation. When anxiety spikes, using TIPP can quickly bring the nervous system back to baseline.
- Grounding techniques (somatic experiencing) – When flashbacks or dissociation hit, anchoring in the present moment helps veterans regain control. A simple exercise like 5-4-3-2-1 grounding (naming five things you see, four things you feel, three things you hear, two things you smell, and one thing you taste) keeps them connected to reality.
- Defusion (ACT) – PTSD makes painful thoughts feel absolute, but defusion techniques help veterans detach from them. Instead of saying “I am broken,” shifting to “I am having the thought that I am broken” creates space between the thought and reality, making it easier to move forward.
Coping skills only work if they become part of daily life. At The Last Resort Recovery, we help veterans integrate these strategies so they feel prepared to manage triggers, regulate emotions, and reclaim their lives.
What to Do When Someone with Complex PTSD Pushes You Away
Supporting a veteran with complex PTSD (CPTSD) can be even more challenging than supporting someone with traditional PTSD. CPTSD develops after prolonged exposure to trauma—such as repeated combat experiences, military sexual trauma, or childhood adversity—leading to deep-seated difficulties with trust, emotional regulation, and self-worth. Unlike PTSD, which is often linked to a single traumatic event, CPTSD involves a broader pattern of emotional and relational struggles.

Recent research suggests that CPTSD may be even more common than PTSD in veteran populations. A systematic review of military and veteran studies found that CPTSD prevalence ranged from 5% to 80.63%, compared to PTSD rates of 3.8% to 42.37%.[5] The wide range reflects differences in study populations, but the trend is clear—many veterans experience chronic, complex trauma that requires specialized support.
When a veteran with CPTSD pushes you away, it’s often an automatic defense mechanism rather than a reflection of how they feel about you. Here’s how you can respond:
- Give Them Space, But Stay Present – Let them know you’re there without pressuring them to engage. A simple “I’m here for you when you’re ready” can go a long way.
- Don’t Take It Personally – Their withdrawal isn’t about you but their internal battle. Avoid reacting with anger or frustration, even if it’s painful.
- Set Boundaries – While being supportive is important, it’s okay to set limits on how much emotional weight you can carry. Make sure you’re taking care of yourself, too.
- Encourage Professional Help – If they’re open to it, gently suggest resources or therapy that could help. If they’re resistant, plant the seed without forcing the issue.
- Find Support for Yourself – Supporting someone with PTSD can be emotionally exhausting. Consider seeking a support group or talking to a therapist who specializes in trauma.
At The Last Resort Recovery, we help veterans rebuild trust, navigate emotional regulation, and develop healthier ways to engage with their loved ones. Healing takes time, but meaningful progress is possible with the right support system.
How Does PTSD Affect Veterans’ Relationships?
PTSD doesn’t just affect the veteran—it affects everyone around them. Relationships with partners, family members, and friends can become strained when PTSD symptoms make communication, trust, and emotional connection difficult. Some of the most common challenges include:

- Emotional Numbness – Veterans with PTSD often struggle to feel emotions the same way they used to. This can lead to detachment, making it hard for them to express love, joy, or connection in relationships.
- Irritability & Anger – PTSD can cause heightened stress responses, leading to quick tempers, emotional outbursts, or difficulty handling conflict. Even minor frustrations can trigger a fight-or-flight reaction.
- Avoidance of Intimacy – Many veterans withdraw from loved ones, either physically or emotionally, to protect themselves from vulnerability or feeling “weak.” This can create distance in romantic relationships and friendships.
- Trust Issues – PTSD can make it hard for veterans to trust others, even those closest to them. This can stem from past experiences in the military where trust was broken or survival depended on being constantly alert to danger.
- Guilt & Shame – Some veterans feel that their trauma makes them “broken” or undeserving of love. These feelings can lead to self-sabotage in relationships, where they push others away before they can be abandoned.
Despite these challenges, strong relationships can survive PTSD with the proper support and communication. Encouraging open conversations, seeking professional help, and practicing patience can help veterans rebuild connection and trust. At The Last Resort Recovery, we provide therapy that helps veterans strengthen their relationships, teaching them how to navigate emotional barriers and reconnect with the people who matter most.
Why Specialized PTSD Treatment Matters
Many veterans find that traditional therapy alone isn’t enough to address the complexities of PTSD. The experiences they carry from military service often require a treatment approach that goes beyond talk therapy. They need a program that understands the realities of service-related trauma and offers practical, hands-on ways to heal. Without this kind of specialized support, many veterans struggle to make meaningful progress in their recovery.

Many of the veterans who come to The Last Resort Recovery have tried traditional therapy without success. Our specialized approach—blending trauma therapy with experiential treatments—helps them engage in healing in a way that resonates with their experiences and needs.
1. Trauma-Focused Therapy
Veterans with PTSD need therapy that directly addresses the impact of trauma on their thoughts, emotions, and behaviors. That’s why we use cognitive processing therapy (CPT), prolonged exposure therapy (PE), and eye movement desensitization and reprocessing (EMDR)—all proven methods that help veterans reprocess their experiences more healthily. These therapies work by breaking the cycle of avoidance, assisting veterans to confront and reframe painful memories so they no longer hold power over their lives.
2. Equine-Assisted Therapy
For many veterans, trust is a significant barrier to healing. Working with horses provides a unique way to rebuild trust and develop emotional awareness in a non-judgmental space.

Equine-assisted therapy fosters connection, patience, and a sense of responsibility, helping veterans learn to regulate their emotions and respond to challenges in a healthier way. Many who struggle to express their feelings in traditional therapy find that interacting with horses provides a breakthrough in their healing journey.
3. Fitness & Outdoor Activities
Physical activity is a powerful tool for managing PTSD symptoms, reducing stress, and improving mental clarity. The Last Resort Recovery incorporates fitness therapy and outdoor experiences as key recovery components.

Whether hiking, strength training, or participating in structured recreational activities, movement helps veterans release built-up tension and regain control over their bodies and minds. Spending time outdoors also offers a natural grounding, allowing veterans to reset in a peaceful, open environment.
4. Peer Support & Brotherhood
Healing is more straightforward when surrounded by people who understand what you’ve been through. Our male-only program creates a strong sense of brotherhood, allowing veterans to connect with others who share similar experiences.

Many veterans feel isolated in their struggles, but at The Last Resort Recovery, they build relationships with peers who truly “get it.” This shared experience fosters trust, accountability, and support—key elements in long-term recovery.
5. Outpatient Treatment for Long-Term Recovery
Recovery from PTSD doesn’t end when residential treatment is over—it’s a lifelong process that requires ongoing support and structure. That’s why The Last Resort Recovery offers a comprehensive continuum of care, including our partial hospitalization (PHP) and intensive outpatient programs (IOP), allowing veterans to continue healing while maintaining daily responsibilities.
We’ve seen how veterans in our Austin-based outpatient program benefit from the flexibility to continue working and staying connected to their families while receiving intensive treatment. This balance allows them to apply coping skills in real-world situations while still having structured support.
Learn More About Our Levels of Care
Your Support Makes a Difference
Helping a veteran with PTSD isn’t about having all the answers—it’s about being there for them in ways that matter. Small actions, patient listening, and connecting them with the right resources can significantly impact them.

If you or a loved one is struggling, we’re here to help.
Healing is possible, and no veteran should have to face PTSD alone.
Contact us today to learn more about our programs for men at (512) 750-6750.